Abstract
Background
Graft versus host disease (GVHD) of the gut is associated with significant morbidity and mortality risk after allogeneic hematopoietic cell transplant (allo-HCT). Endoscopy and biopsies of the gut mucosa is recommended to confirm the clinical findings of gut GVHD and to rule out infectious etiologies. There is paucity of data to guide when to repeat endoscopy after inconclusive findings of first endoscopy or after failure of first line treatment with steroids. We aimed to study if repeat biopsy is helpful in these patients for treatment decisions.
Methods
In this study, we retrospectively reviewed medical records of all patients who underwent endoscopies twice for clinical suspicion of GI GVHD after undergoing allo-HCT between 2012 to 2016 at University of Iowa. Demographic, disease, allo-HCT characteristics as well as endoscopic and histological findings during first and second endoscopies were extracted from medical records. We sought to identify if any findings on second endoscopy led to changes in the clinical management of these patients. Additionally, we documented if repeat endoscopy led to any complications.
Results
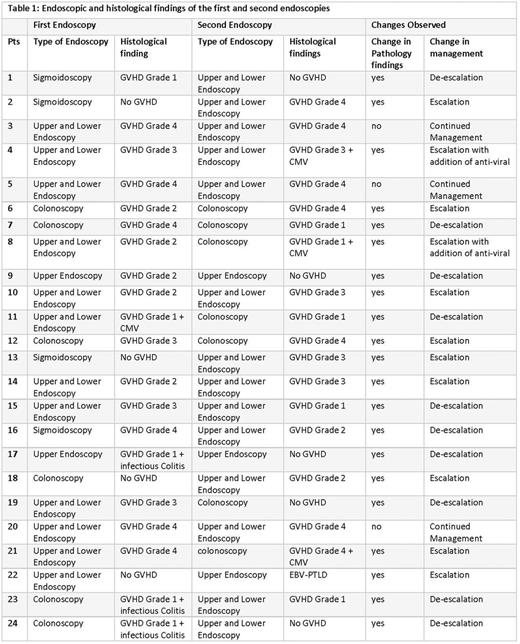
Of the 318 patients (pts) reviewed, 24 pts underwent endoscopy twice after allotransplant for clinical suspicion of GVHD. Median age (range) was 55 (18-72) years and 13 pts were male. The most common diagnosis was myelodysplastic syndrome (n=10), followed by acute myelogenous leukemia (n=7), acute lymphoblastic leukemia (n=4), Non-Hodgkin lymphoma (n=2) and Chronic myelogenous leukemia (n=1). HLA matched unrelated donor (n=13) was the most common type of transplant followed by HLA matched related donor (n=5), HLA mismatched -unrelated donor (n=5) and one was cord blood transplant. The most common GVHD prophylaxis used was Tacrolimus + methotrexate (n=17), followed by Tacrolimus + Mycophenolate Mofetil (n=7). At the time of first endoscopy 6 pts had only a colonoscopy, 4 pts had sigmoidoscopy, 2 had only upper endoscopy and 12 pts had both upper and lower endoscopy. At first endoscopy 20 pts (80%) showed abnormal findings that included 16 pts with GVHD alone, 1 pt with GVHD and CMV, and 3 pts with GVHD and infectious colitis. The remaining 4 pts had normal endoscopic findings on first endoscopy (2 underwent sigmoidoscopies, 1 colonoscopy, and 1 upper and lower endoscopy). On repeat colonoscopy in these 4 pts with normal first investigation, (3 underwent upper and lower endoscopies and one upper endoscopy on repeat procedure) 3 pts were found to have GVHD and 1 pt had EBV-PTLD. Among the 20 pts who had histological evidence of GVHD on initial endoscopy, 6 pts exhibited improvement in histological findings leading to de-escalation of therapy, 8 pts showed worsening histological findings of GVHD and 2 showed presence of CMV resulting in significant change in management (escalation of therapy), 2 pts had no histological changes. One pt who had initial histological findings of GVHD and CMV displayed significant improvement leading to de-escalation of therapy. Three pts with GVHD along with infectious colitis on biopsy subsequently showed improvement on repeat biopsy leading to de-escalation of therapy. Overall, no complications of repeating the procedures were noted. The endoscopic and histological findings of the first and second endoscopies are shown in Table 1.
Conclusion
This study supports the utility of repeat endoscopy in persistently symptomatic patients when there is no improvement with initial treatment based on the results of the first endoscopy. Additionally, repeat endoscopy can guide both escalation and de-escalation of therapy in this patient population without any significant complications or side effects.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal